Spinal stenosis occurs when the space within the spine becomes too narrow, which can put pressure on the spinal cord and the nerves that pass through it. It most commonly affects the lower back and the neck. Some individuals with spinal stenosis may not have any symptoms, while others may experience pain, tingling, numbness, or muscle weakness. These symptoms may worsen over time. The leading cause of spinal stenosis is degeneration in the spine due to arthritis. In severe cases, surgery may be required. Surgery can increase space in the spine, relieving pressure on the spinal cord or nerves, but it won’t treat arthritis itself, so arthritis-related back pain may persist.
What is spinal stenosis?
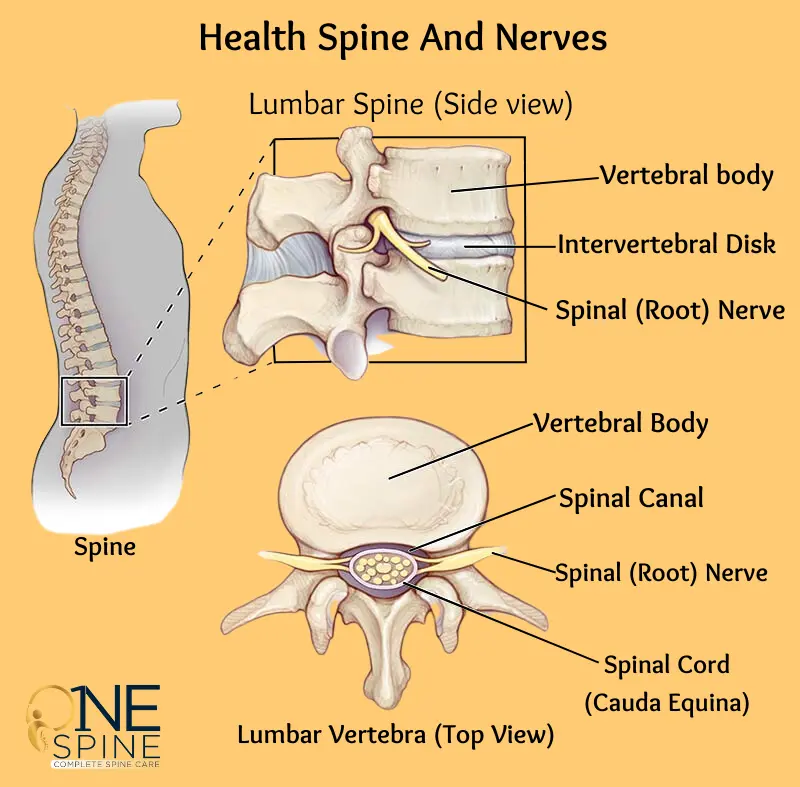
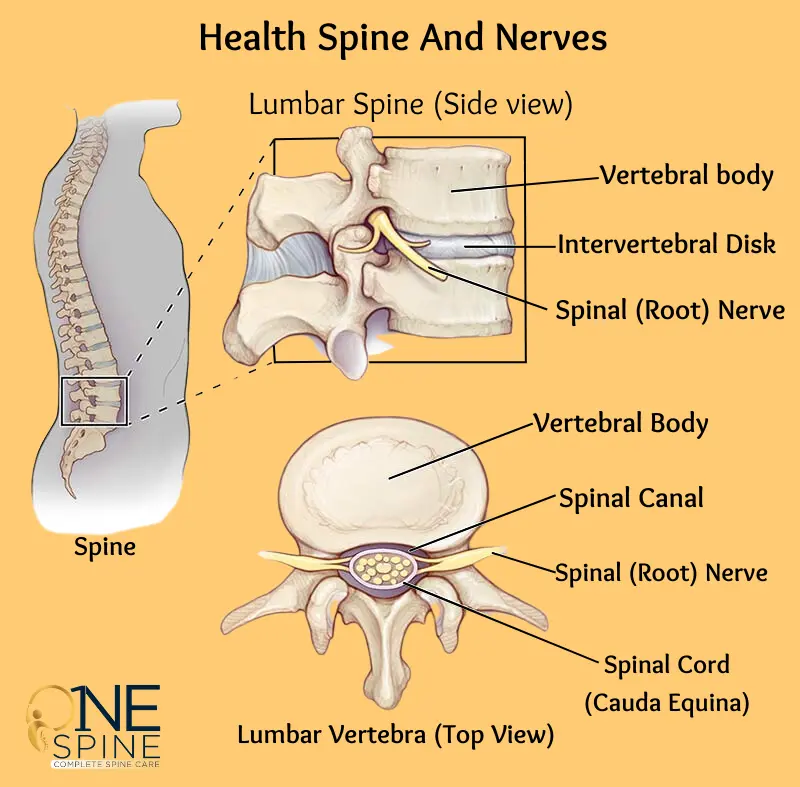
Spinal stenosis is a condition where one or more spaces within the spinal canal become narrowed. The spinal canal is a passageway that runs through each vertebra in the spine and houses the spinal cord. When the space within the canal decreases, it puts pressure on the spinal cord and the nerves that branch off from it (nerve roots).
This narrowing can irritate, compress, or pinch the spinal cord or nerves, leading to symptoms like back pain and nerve-related issues such as sciatica. Several factors, including certain conditions and injuries, can contribute to a narrowed spinal canal.
While spinal stenosis can affect anyone, it is most commonly seen in individuals over the age of 50.
The two areas of the spine most commonly affected by spinal stenosis are:
- Lower back (lumbar spinal stenosis): The lumbar spine consists of five vertebrae (L1 to L5) in the lower back. These are the largest vertebrae in the entire spine.
- Neck (cervical spinal stenosis): The cervical spine consists of seven vertebrae (C1 to C7) in the neck.
Although spinal stenosis can occur in the middle back (thoracic spine), it is rare.
How common is spinal stenosis?
Spinal stenosis is relatively common, particularly as people age. Degenerative changes in the spine affect up to 95% of individuals by the age of 50, and spinal stenosis is one of those changes. Among people over 65 who undergo spine surgery, lumbar spinal stenosis is the most frequent diagnosis.
Symptoms and Causes of Spinal Stenosis
What are the symptoms of spinal stenosis?
Spinal stenosis can manifest a variety of symptoms depending on its location and severity. These symptoms may affect different parts of the body, including the neck, back, arms, legs, hands, and feet. Common symptoms include:
- Pain: This can vary in intensity and may be localized or radiate to other areas.
- Numbness: A loss of sensation may occur in the affected areas.
- Tingling: Many individuals report a “pins and needles” sensation.
- Weakness: A decrease in strength can affect mobility and function.
The development of spinal stenosis is usually gradual, which means symptoms might not appear immediately. Even if imaging tests, such as X-rays or MRIs, indicate narrowing in the spinal canal, you may be asymptomatic for some time. Symptoms can be episodic, meaning they may come and go, and they can differ significantly from person to person.
Symptoms of lumbar spinal stenosis
When spinal stenosis occurs in the lumbar region (lower back), it often presents specific symptoms, including:
- Low Back Pain: This is a common complaint and can vary from mild discomfort to severe pain.
- Radiating Pain: Pain may start in the buttocks and extend down one or both legs, sometimes reaching the foot. This pain is often referred to as “sciatica.”
- Heavy Legs: Individuals might experience a feeling of heaviness in the legs, which can be accompanied by cramping, especially during physical activity.
- Numbness or Tingling: Sensations of numbness or tingling (often described as “pins and needles”) may occur in the buttocks, legs, or feet.
- Activity-Dependent Pain: Symptoms often worsen with prolonged standing, walking, or walking downhill. Conversely, symptoms may improve when leaning forward, walking uphill, or sitting down.
These symptoms can significantly impact daily activities and may necessitate changes in lifestyle or behavior to manage discomfort.
Symptoms of cervical spinal stenosis
Cervical spinal stenosis affects the neck region and can lead to symptoms that manifest below the point of nerve compression. These symptoms may include:
- Neck Pain: Pain in the neck can range from mild to severe and may radiate to other areas.
- Numbness or Tingling: Patients may feel numbness or tingling in the arms, hands, legs, or feet, depending on which nerves are affected.
- Weakness or Clumsiness: This can result in difficulty performing everyday tasks, such as gripping objects or holding utensils.
- Balance Problems: Some individuals may experience difficulties with balance, leading to an increased risk of falls.
- Decreased Hand Function: This can manifest as challenges in fine motor skills, making activities like writing or buttoning shirts difficult.
What does spinal stenosis pain feel like?
The nature of pain associated with spinal stenosis can vary significantly among individuals. Some people describe the pain as a dull, aching sensation, while others report sharper, electric-like or burning feelings. The pain may not be constant; it can fluctuate based on activity levels, posture, and other factors.
Understanding these symptoms is crucial for early detection and management of spinal stenosis. If you experience any of these symptoms, particularly if they interfere with daily activities or worsen over time, it’s advisable to consult a healthcare professional for further evaluation and potential treatment options.
What causes spinal stenosis?
Spinal stenosis can arise from various factors, leading to a narrowing of the spinal canal. The causes can be categorized into two primary groups:
- Acquired (developing after birth)
- Congenital (present from birth)
Acquired spinal stenosis is more prevalent, often resulting from age-related changes or injuries to the spine. In fact, only about 9% of cases stem from congenital causes.
Acquired causes of spinal stenosis
Acquired spinal stenosis typically develops later in life, usually after the age of 50. This condition often results from degenerative changes in the spine associated with aging or specific injuries. Key causes include:
- Bone Overgrowth: Osteoarthritis, a common degenerative condition, leads to the breakdown of cartilage in the joints, including those in the spine. As the protective cartilage wears away, the underlying bones can rub against each other, prompting the body to respond by producing new bone growth. This process can result in the formation of bone spurs, which extend into the spinal canal and narrow the available space, potentially pinching the nerves. Conditions like Paget’s disease can also contribute to excessive bone growth in the spine.
- Bulging or Herniated Disks: The vertebral disks serve as shock absorbers between the vertebrae. With age, these disks may dry out and flatten, leading to cracks in their outer layers. When the gel-like center of the disk protrudes through these cracks (a herniated disk), it can press on nearby nerves, causing pain and discomfort.
- Thickened Ligaments: Ligaments are tough, fibrous bands that stabilize the spine. Conditions like arthritis can lead to thickening of these ligaments over time, causing them to bulge into the spinal canal and further narrow the space available for the spinal cord and nerves.
- Spinal Fractures and Injuries: Traumatic injuries or fractures to the vertebrae can directly reduce the size of the spinal canal. Inflammation resulting from these injuries can also exacerbate narrowing and contribute to discomfort.
- Spinal Cysts or Tumors: Abnormal growths within or around the spinal cord or vertebrae can create pressure on the spinal canal, leading to stenosis.
Congenital causes of spinal stenosis
Congenital spinal stenosis is present at birth and can affect infants and children. This condition may arise due to:
- Abnormalities in spine formation during fetal development.
- Genetic conditions that interfere with normal bone growth, often resulting from specific genetic mutations.
Some congenital causes include:
- Achondroplasia: A genetic disorder affecting bone growth, leading to dwarfism and an increased risk of spinal stenosis.
- Spinal Dysraphism: A group of conditions where the spine, spinal cord, or nerve roots do not develop properly during fetal development. Examples include spina bifida and other neural tube defects.
- Congenital Kyphosis: This occurs when the spine curves outward excessively, resulting in an overly rounded upper back due to developmental issues in the fetus.
- Congenital Short Pedicles: When infants are born with shorter vertebral pedicles (the bony sides of the spinal canal), this can decrease the size of the spinal canal.
- Osteopetrosis: A rare genetic condition that leads to abnormal bone density and growth, potentially contributing to spinal stenosis.
- Morquio Syndrome: A rare genetic disorder affecting bone, spine, and other body systems, leading to potential narrowing of the spinal canal.
- Hereditary Multiple Exostoses (Diaphyseal Aclasis): A rare genetic condition that results in the growth of multiple bony protrusions on the vertebrae, which can narrow the spinal canal.
Understanding the various causes of spinal stenosis is essential for effective diagnosis and treatment. If you experience symptoms associated with spinal stenosis, it is crucial to consult a healthcare professional for evaluation and appropriate management.
Diagnosis and Tests of Spinal Stenosis
How is spinal stenosis diagnosed?
Diagnosing spinal stenosis involves a comprehensive evaluation by your healthcare provider. The process typically begins with a thorough review of your medical history, where the provider will inquire about your symptoms, their onset, and any factors that may alleviate or exacerbate them.
During the physical examination, the provider may palpate (feel) different areas of your spine to identify any points of tenderness or pain. You may also be asked to perform specific movements, such as bending or twisting, to determine if these positions trigger symptoms.
In addition to the physical exam, your provider will likely recommend imaging tests to obtain a clearer view of your spine and pinpoint the location and severity of the stenosis. Common imaging tests used in the diagnosis of spinal stenosis include:
- Spine X-ray: X-rays utilize a small amount of radiation to create images of your spine. They are effective in visualizing changes in bone structure, such as loss of disk height, bone spurs, or any other bony abnormalities that may contribute to narrowing of the spinal canal.
- Magnetic Resonance Imaging (MRI): An MRI uses powerful magnets and radio waves to generate detailed cross-sectional images of your spine. This imaging technique provides a comprehensive view of soft tissues, including nerves, disks, and the spinal cord. MRI is particularly useful for detecting any tumors, herniated disks, or other conditions that may be contributing to the symptoms of spinal stenosis.
- Computed Tomography (CT) Scan or CT Myelogram: A CT scan combines multiple X-ray images taken from different angles to produce cross-sectional views of your spine. This can provide additional detail on the bone structures of the spine. A CT myelogram enhances this process by injecting a contrast dye into the spinal canal, allowing for clearer visualization of the spinal cord and nerve roots. This can be especially helpful in identifying areas of compression.
Together, these diagnostic methods enable your healthcare provider to accurately assess the extent of spinal stenosis and develop an appropriate treatment plan tailored to your needs. If spinal stenosis is diagnosed, your provider will discuss various treatment options, which may include physical therapy, medication, or, in more severe cases, surgical intervention.
Management and Treatment Of Spinal Stenosis
What is the treatment for spinal stenosis?
The treatment for spinal stenosis varies based on several factors, including:
- The underlying cause of the condition.
- The specific location of the stenosis within the spine.
- The severity and impact of your symptoms on daily life.
For individuals experiencing mild symptoms, healthcare providers often recommend conservative at-home care as the first step. If these initial measures prove ineffective and symptoms worsen, additional treatments may include physical therapy, medication, injections, and potentially surgery as a last resort.
At-home care for spinal stenosis
At-home care strategies can help alleviate symptoms and improve quality of life. These may include:
- Applying Heat: Heat therapy can be beneficial for easing discomfort associated with osteoarthritis, as it promotes increased blood flow, relaxes tight muscles, and alleviates joint stiffness. However, care should be taken to avoid burns from excessive heat.
- Applying Cold: If heat does not provide relief, ice therapy can be effective. Ice packs, frozen gel packs, or even a bag of frozen peas can be applied to the affected area for 20 minutes on and 20 minutes off. Cold therapy helps reduce swelling and inflammation while numbing the pain.
- Exercising: Engaging in gentle exercise can be beneficial for spinal stenosis. Consult with your healthcare provider before starting any exercise regimen. Regular physical activity can strengthen the muscles that support the spine, improve flexibility, and enhance balance, ultimately relieving discomfort.
Nonsurgical treatment for spinal stenosis
Nonsurgical treatments primarily aim to manage the symptoms associated with spinal stenosis. These options may include:
- Oral Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce inflammation and relieve pain. It’s important to consult your healthcare provider regarding the potential long-term effects of these medications. In some cases, your provider may recommend prescription medications that have pain-relieving properties, such as gabapentin (an antiseizure medication) or tricyclic antidepressants like amitriptyline. Muscle relaxants can also be beneficial for addressing cramps or spasms.
- Physical Therapy: Physical therapists can develop personalized exercise programs to strengthen your back and core muscles, enhancing stability and resilience. They can also teach you techniques to adjust your posture and movement, helping to alleviate pressure on your spinal nerves.
- Steroid Injections: Corticosteroid injections can be administered around the affected spinal nerves to reduce inflammation, pain, and irritation, providing temporary relief.
Surgery for spinal stenosis
Surgery for spinal stenosis is generally considered only after conservative treatment options have been exhausted. Most individuals with spinal stenosis do not require surgical intervention, but for those who do, several surgical options are available:
- Laminectomy (Decompression Surgery): This is the most frequently performed surgery for spinal stenosis. The procedure involves removing the lamina, a bony section of the vertebra, to create more space for the spinal cord and nerves. In some cases, the surgeon may also remove bone spurs or ligaments that contribute to nerve compression.
- Laminotomy: A laminotomy involves a partial removal of the lamina, specifically targeting the area that is pressing against the nerve roots.
- Laminoplasty: This surgery is specifically for cervical spinal stenosis. The surgeon removes part of the lamina to widen the spinal canal and then uses metal plates and screws to create a hinged structure across the area.
- Foraminotomy: This procedure focuses on the foramen, the openings in the vertebrae through which nerve roots exit. Bone or tissue is removed to increase the available space for the nerve roots.
- Interspinous Process Spacers: A minimally invasive procedure for lumbar spinal stenosis, this involves inserting spacers between the spinous processes (bony protrusions on the back of each vertebra). This technique aims to maintain separation between vertebrae, thus creating more space for the nerves.
- Spinal Fusion: Spinal fusion is typically reserved for patients with severe symptoms, particularly radiating nerve pain, or for those whose spine is unstable and has not responded to other treatments. This surgery permanently fuses two vertebrae together, which can help stabilize the spine.
Selecting the appropriate treatment for spinal stenosis requires a thorough evaluation and discussion with your healthcare provider to ensure the best approach for your specific situation.
Prevention of Spinal Stenosis
Can I prevent spinal stenosis?
While it’s not possible to entirely prevent spinal stenosis, as many of its causes are related to age and natural degeneration, there are several proactive measures you can take to promote spinal health. These strategies can help reduce your risk or slow the progression of spinal stenosis. Here are some effective steps you can consider:
- Eating a Nutrient-Rich Diet: Focus on a balanced diet that includes plenty of calcium and vitamin D to support bone health. Foods such as dairy products, leafy greens, and fortified cereals can help strengthen your bones and prevent conditions that may lead to spinal issues. Additionally, a diet rich in fruits, vegetables, and whole grains provides essential nutrients that can help reduce inflammation.
- Maintaining a Healthy Weight: Excess body weight puts additional strain on your spine and can contribute to the development of spinal stenosis. By maintaining a healthy weight through a balanced diet and regular physical activity, you can reduce the pressure on your spine and lower your risk of degenerative changes.
- Avoiding Tobacco Products: Smoking has been shown to negatively impact circulation and overall health. It can harm your arteries, leading to reduced blood flow and oxygen delivery to your spine. This can hinder the healing process and increase the risk of developing back pain. If you smoke, seeking support to quit can significantly benefit your spinal health.
- Practicing Good Posture: Maintaining proper posture while sitting, standing, and lifting can help reduce unnecessary stress on your spine. Be mindful of your alignment, keeping your back straight and shoulders back. Ergonomic furniture and tools can also assist in promoting good posture in your daily activities.
- Engaging in Regular Exercise: Regular physical activity is crucial for maintaining strong muscles, particularly those in your back and core. Exercises that focus on strength, flexibility, and balance—such as swimming, walking, or yoga—can support spinal health. Aim for at least 150 minutes of moderate aerobic activity each week, along with strength-training exercises on two or more days.
Incorporating these lifestyle changes can help keep your spine healthy and may potentially delay or reduce the risk of developing spinal stenosis. Regular check-ups with your healthcare provider can also ensure early detection and management of any spinal issues that may arise.
Thanks For Read